TLDR;
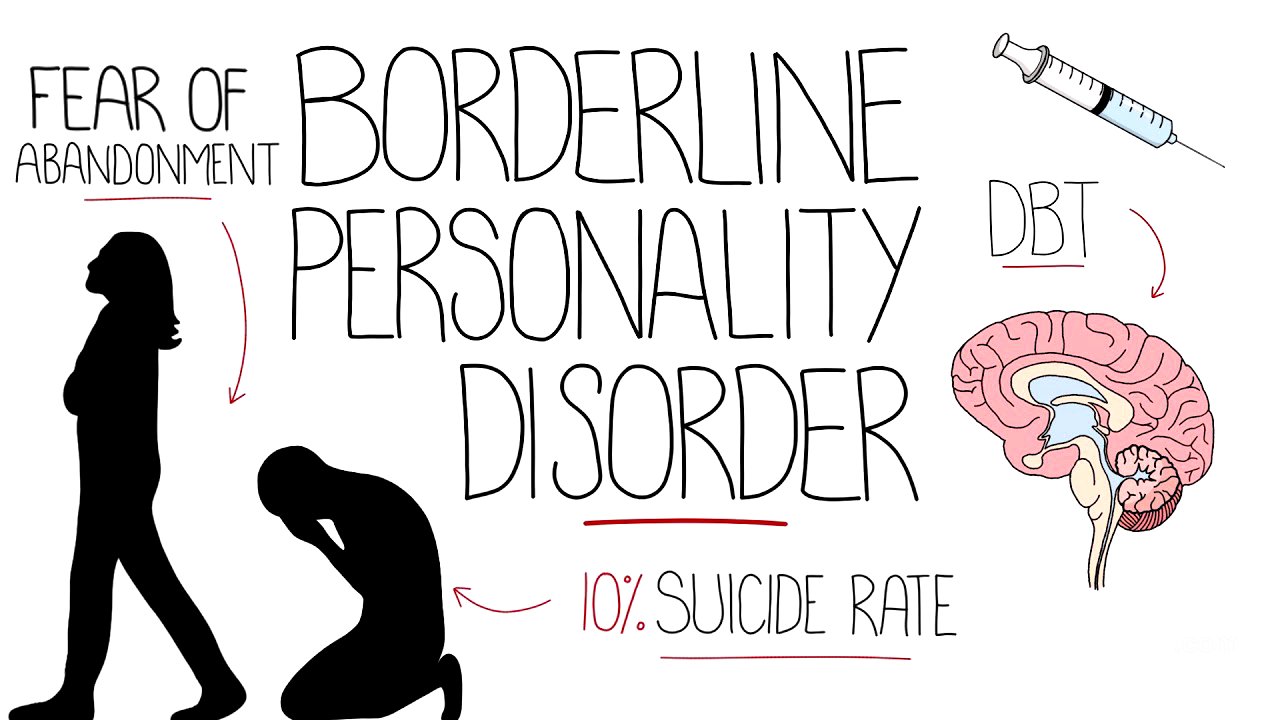
This video provides an overview of Borderline Personality Disorder (BPD), covering its definition, diagnostic criteria, symptoms, prevalence, causes, associated risks, and treatment options. It highlights the core symptoms, including fear of abandonment, unstable relationships, and impulsivity, and discusses the importance of psychotherapy in managing the disorder.
- BPD is characterized by strong emotional responses, unstable relationships, and a distorted sense of self.
- Diagnosis requires the presence of at least five out of nine core symptoms.
- Treatment primarily involves psychotherapy, with specific therapies like mentalizing-based therapy and dialectical behavior therapy.
Introduction to Borderline Personality Disorder [0:05]
The video introduces Borderline Personality Disorder (BPD) as a condition where an individual's personality deviates significantly from societal norms, leading to impaired functioning. BPD, classified as a cluster B disorder, is characterized by intense emotional reactions, unstable interpersonal relationships, and a distorted self-perception. In the ICD classification, it is referred to as emotionally unstable personality disorder.
Core Signs and Symptoms of BPD [0:45]
The nine core symptoms of BPD include a fear of abandonment, which can be real or perceived, leading to frantic efforts to avoid it. People with BPD often experience unstable relationships, with feelings towards others shifting rapidly between idealization and devaluation, a phenomenon linked to splitting, where individuals are seen as either entirely good or entirely bad. Other symptoms include a disturbed sense of identity, impulsivity (e.g., unsafe sex, substance abuse), recurrent suicidal thoughts or self-harm, emotional dysregulation, feelings of emptiness, uncontrollable anger, and severe dissociation or stress-related paranoia.
Diagnostic Criteria and Prevalence [1:50]
To meet the DSM-5 criteria for BPD, an individual must exhibit at least five of the nine listed symptoms across various contexts. The disorder is typically diagnosed in early adulthood but can be identified in individuals under 18. BPD is believed to arise from a combination of genetic, environmental, and social factors. It affects approximately one to two percent of the general population and twenty percent of the inpatient psychiatry population. While studies have previously indicated a higher female to male ratio in clinical settings, the prevalence appears roughly equal when considering the general population.
Etiology and Risk Factors [2:36]
The heritability of BPD is estimated to be up to 69%, indicating a significant genetic component, as supported by twin studies. However, these results may be influenced by the similar environments shared by twins. A strong correlation exists between childhood abuse (emotional, physical, and sexual) and unstable family environments and the development of BPD. Approximately 70% of patients with BPD report a history of abuse or neglect.
Associated Risks and Comorbidities [3:12]
BPD can significantly impair an individual's ability to complete education and maintain employment. Risky behaviors, such as unsafe sex and reckless driving, are common and increase the risk of harm. Overall, 10% of patients with BPD die by suicide. Comorbidity is high, with 80-96% of BPD patients also experiencing mood disorders, 88% anxiety disorders, 64% substance abuse, 53% eating disorders, 10-30% attention deficit hyperactivity disorder, and 15% bipolar disorder.
Treatment Options for BPD [3:57]
Currently, no medication is specifically approved for BPD, although certain classes of drugs, such as anti-convulsants, antidepressants, anxiolytics, and antipsychotics, are sometimes prescribed to manage symptoms. Psychotherapy, or talking therapy, is the primary treatment approach. Three main therapies are particularly effective: mentalizing-based therapy, which helps manage emotional dysregulation and fosters understanding by reducing assumptions about others' intentions; dialectical behavior therapy, which uses interpersonal skills and mindfulness to achieve emotional regulation and reduce conflict in relationships; and transference focused psychotherapy, which raises the patient’s awareness of interpersonal issues and self-destructive behaviors.