TLDR;
This lecture provides an overview of rehabilitation strategies for common sports injuries. It emphasizes the importance of structured, progressive programs to restore function, reduce pain, and ensure a safe return to activity. Key aspects covered include the goals and phases of rehabilitation, principles of rehabilitation, specific injury rehabilitation protocols, screening and neuromuscular training, the roles of orthotics, nutrition, and psychology, and future trends in rehabilitation.
- Rehabilitation is crucial for regaining strength, flexibility, coordination, and confidence after a sports injury.
- A multidisciplinary approach involving sports physicians, physiotherapists, nutritionists, and psychologists is essential for effective rehabilitation.
- Future trends include technological advancements like wearable tech, AI-driven programs, virtual reality, and regenerative medicine.
Introduction [0:15]
The lecture introduces rehabilitation scenarios for common sports injuries, outlining the topics to be covered. These include the goals and phases of rehabilitation, principles of rehabilitation, rehabilitation for common injuries, screening and neuromuscular training, the roles of orthotics, nutrition, and psychology in rehab, future trends, and a concluding take-home message. The lecture emphasizes that each injury could be a topic in itself, and the aim is to provide a general outline of rehabilitation strategies.
Goals and Phases of Rehabilitation [1:33]
Rehabilitation is defined as a structured, progressive program designed to restore function, reduce pain, and facilitate an athlete's safe return to activity. It is important because it helps athletes regain strength, flexibility, and coordination, and it restores their confidence after an injury. The goals of rehabilitation include restoring joint mobility and muscle strength, preventing reinjury through proper movement patterns and conditioning, ensuring a safe return to sport-specific activities, and addressing the psychological aspects of injury recovery. The phases of rehabilitation include the acute phase (immediate post-injury care, pain control, and inflammation management), the subacute phase (controlled movement, progressive strength training, and neuromuscular retraining), and the functional recovery phase (advanced strength training, agility drills, and return-to-play preparation). These phases require a team effort involving sports physicians, PMR specialists, physiotherapists, athletic trainers, nutritionists, psychologists, and SNC coaches.
Principles of Rehabilitation [3:42]
Rehabilitation should be an individualized approach based on the severity and type of injury. It should involve a gradual progression of exercises and good pain management strategies. Real-time daily monitoring for complications is necessary, and rehabilitation is always a multidisciplinary approach. The soft tissue healing process includes an inflammatory phase (0-7 days) with pain, swelling, and redness; a proliferation phase (7-21 days) with tissue regeneration and scar formation; and a remodeling phase (3 weeks to months) where new tissue gradually strengthens. Controlled movement plays a role in each phase to facilitate healing.
Rehabilitation for Common Injuries [5:10]
The lecture outlines rehabilitation strategies for various common sports injuries. For ankle sprains, Phase 1 involves the POLICE or RICE protocol, pain control, and immobilization if severe. Phase 2 includes range of motion exercises and balance training, while Phase 3 focuses on strengthening, proprioception drills, and sports-specific activities. ACL injuries require prehabilitation (quadriceps and hamstring strengthening) to minimize atrophy, followed by post-surgery gradual weight-bearing, controlled motion, and early neuromuscular training. The final phase includes plyometric training, agility work, and cutting drills. Hamstring strains involve early-stage rest and pain control, Nordic hamstring curls for eccentric strengthening, running drills, and addressing muscle imbalances. Shoulder dislocations initially require immobilization, followed by passive range of motion, scapular stabilization, rotator cuff strengthening, and sport-specific biomechanics training. Rotator cuff injuries involve pain control, gentle mobility work, strengthening of the rotator cuff and scapula stabilizers, and functional drills based on the sport's demands. Achilles tendinopathy rehabilitation includes eccentric loading exercises, biomechanical corrections, and a gradual return to explosive movements. Stress fractures require immediate load reduction, nutritional support (calcium, vitamin D, protein, vitamin B12, magnesium, and zinc), and a progressive return to activity. Tennis elbow rehabilitation involves range of motion exercises, isometric and eccentric exercises, soft tissue mobilization techniques, and gradual loading of the forearm musculature. Patellar tendinopathy rehabilitation includes isometric exercises to reduce pain, progressive strengthening using isotonic and eccentric exercises, and plyometrics. Groin strains require immediate rest with gentle mobility, core stability, hip strengthening exercises, and sport-specific agility drills. Low back pain in athletes involves immediate rest, core stabilization, postural correction, movement retraining, and a gradual return to impact activities.
Screening and Neuromuscular Training [10:06]
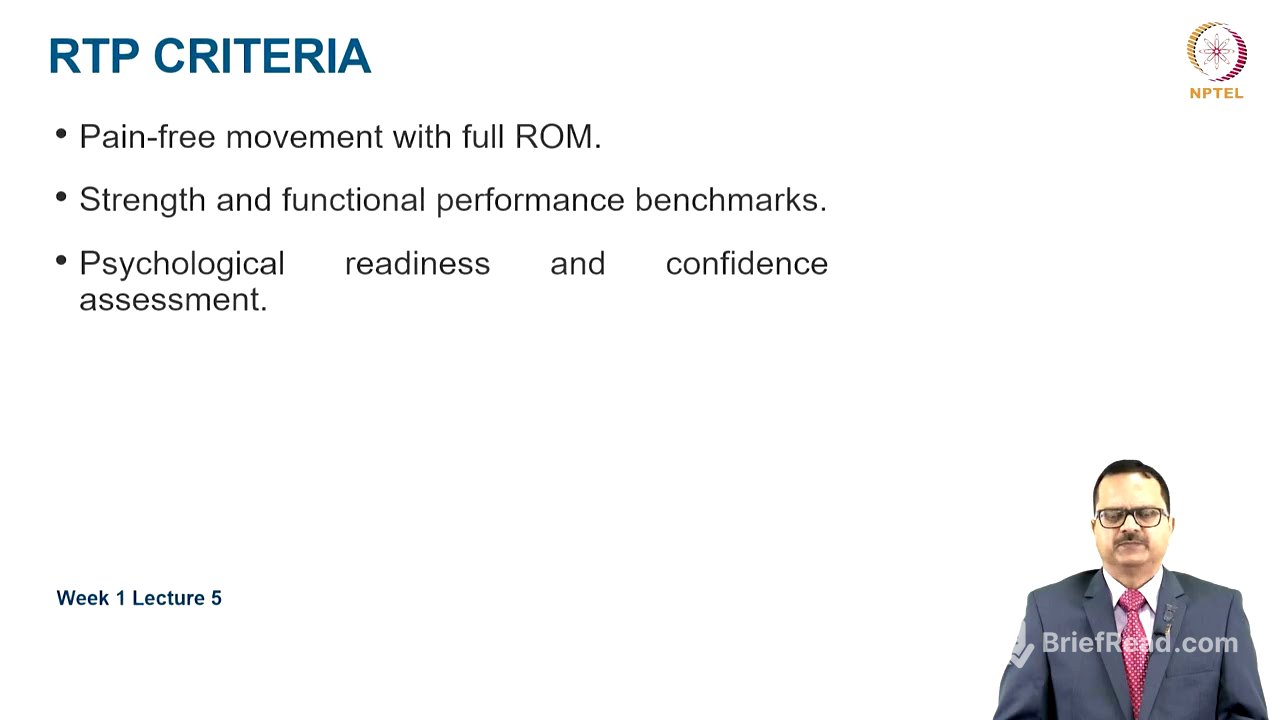
Functional movement screening (FMS) and Y-balance tests are used to identify biomechanical deficits and modify training plans. Neuromuscular training is essential for injury prevention, improving proprioception, balance, and coordination, and it plays a significant role in ACL and ankle injury prevention. Return-to-play criteria include a pain-free joint throughout the full range of motion, achievement of strength and functional performance benchmarks, and the athlete being psychologically ready with a confidence assessment.
Role of Physical Medicine and Rehab, Orthotics, Nutrition and Psychology [11:13]
Physical medicine and rehabilitation (PMR) uses modalities for pain and inflammation reduction and tissue healing, hands-on techniques like mobilization and massage, tailored exercise programs, education on proper movement mechanics, drug therapy, and orthotics prescription. Bracing and taping support unstable joints during rehabilitation and enhance proprioception, but their long-term benefits remain uncertain. Nutrition plays a vital role, with good quality protein for muscle repair, calcium, vitamin D, collagen, vitamin B12, zinc, and magnesium for bone and connective tissue health, proper hydration, and anti-inflammatory diets. Psychological aspects of rehabilitation include managing the fear of reinjury, correct goal setting, motivation techniques, and sport psychology interventions.
Future Trends [13:09]
Technological advances in rehabilitation include wearable technology to track progress, AI-driven rehab programs with personalized exercise plans, and virtual reality for movement retraining and neuroplasticity enhancement. Future trends involve PRP therapy, stem cell therapy, motion capture technology for biomechanical analysis, blood flow restriction (BFR) training to enhance muscle strength with low resistance loads, 3D printed orthotics and prosthetics, telerehabilitation for remote monitoring, and AI and machine learning for predictive modeling and customized recovery plans.
Take-Home Message [14:55]
Rehabilitation is important to restore function, prevent reinjury, and ensure a safe return to sport. It should progress as per the phases of rehabilitation. Functional movement assessments, neuromuscular training, physiotherapy, nutrition, and psychological support are vital for a proper rehab program. A structured and progressive approach is essential for quality sports rehabilitation.