TLDR;
This lecture provides an overview of common soft tissue sports injuries, their management, and prevention. It covers various types of injuries like strains, sprains, contusions, tendinopathies, and bursitis, detailing their causes, symptoms, and immediate care. The lecture also addresses rehabilitation strategies, pain management, return-to-play guidelines, and considerations for special populations like youth and older athletes. Finally, it touches on future trends in soft tissue injury management, including regenerative medicine and AI-driven rehabilitation.
- Soft tissue injuries include damage to muscles, ligaments, and tendons.
- Management strategies involve immediate care (POLICE protocol), rehabilitation, and pain management.
- Return to play requires pain-free function, restored strength, and sport-specific readiness.
Introduction to Soft Tissue Injuries [0:15]
The lecture introduces the topic of common soft tissue sports injuries, defining them as damage to muscles, ligaments, and tendons due to trauma or overuse. These injuries are prevalent among athletes, and effective management is crucial for quick recovery and preventing recurrence. Key management strategies include immediate care, rehabilitation, pain management, and preventive measures.
Types of Soft Tissue Injuries [1:47]
Different types of soft tissue injuries are discussed, including muscle or tendon strains (overstretching or tearing), sprains (ligament injuries), contusions (bruises from blunt trauma), tendinopathies (chronic tendon irritation), and bursitis (inflammation of the bursae). Each type of injury has distinct causes and symptoms that require specific management approaches.
Strains: Muscle and Tendon Injuries [2:32]
Strains involve the overstretching or tearing of muscle or tendon fibres, often caused by sudden acceleration, deceleration, improper warm-up, or muscle fatigue. Symptoms include pain, swelling, bruising, reduced range of motion, and muscle weakness. Immediate care involves the POLICE protocol (Protection, Optimal Loading, Ice, Compression, Elevation) within 24 to 48 hours, followed by gradual stretching and strengthening exercises, massage therapy, and physical therapy for muscle re-education. Prevention includes proper warm-up, strength training, and correct technique.
Sprains: Ligament Injuries [4:03]
Sprains are partial or complete tears of ligaments, commonly affecting the ankle, knee, and wrist. Symptoms include pain, instability, swelling, bruising, and difficulty in weight-bearing. Immediate management involves the POLICE protocol within 48 hours, gentle mobility exercises, strengthening exercises, and bracing or taping for support. Return to play is contingent on passing functional tests and gradual reintegration into sports activities.
Contusions: Bruises [5:17]
Contusions, or bruises, result from direct trauma causing capillary rupture and bleeding under the skin. Symptoms include discoloration, swelling, pain, and stiffness. Management includes the POLICE protocol for the first 48 hours, gentle stretching to maintain range of motion, and pain management with non-steroidal anti-inflammatory drugs. Aggressive massage should be avoided early on to prevent myositis ossificans (bone formation in muscle tissue).
Tendinopathies: Chronic Tendon Issues [6:07]
Tendinopathies are overuse injuries leading to tendon degeneration and inflammation, such as Achilles tendinopathy, patellar tendinopathy, and lateral epicondylitis. Symptoms include a gradual onset of pain, morning stiffness, and thickening of the tendon. Management involves rest to reduce load, progressive strengthening programs with eccentric and isometric exercises, and therapies like shockwave, ultrasound, or dry needling for pain relief. Corticosteroid injections may be used cautiously to avoid tendon rupture.
Bursitis: Inflammation of the Bursae [7:28]
Bursitis is the inflammation of the bursae due to repetitive stress or direct impact. Bursae are fluid-filled sacs that reduce friction around joints, commonly located in the shoulder, knee, and hip. Conditions include subacromial bursitis of the shoulder, prepatellar bursitis of the knee, and trochanteric bursitis of the hip. Symptoms include localised swelling, warmth, tenderness, and pain with movement. Management involves the POLICE protocol, non-steroidal anti-inflammatory drugs, physical therapy to strengthen surrounding muscles, and, in severe cases, corticosteroid injections.
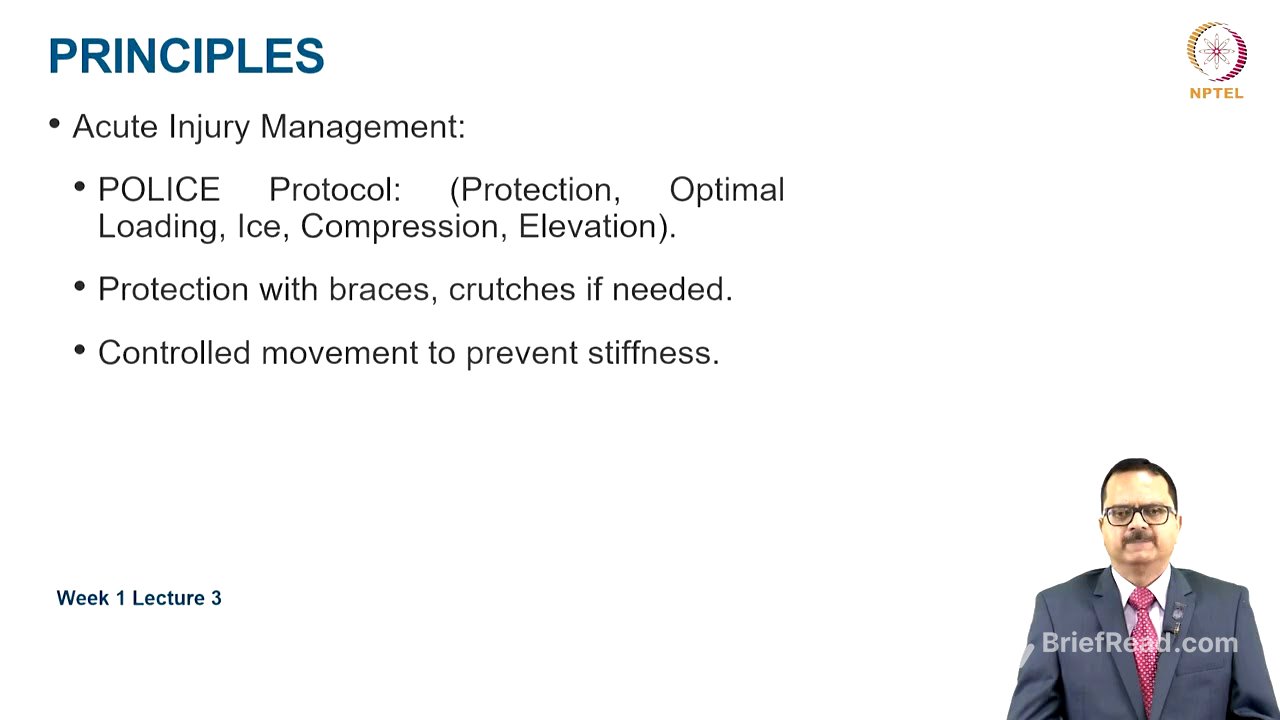
Principles of Soft Tissue Injury Management [8:54]
The principles for acute injury management include the POLICE protocol: protection, optimal loading, ice, compression, and elevation. Protection involves using braces or crutches to rest the damaged tissue, while controlled movement prevents stiffness. The acute phase focuses on reducing pain and swelling, the subacute phase on regaining motion and strength, and the functional phase on sport-specific training. Progressing exercise is more of an art than a science, requiring experience.
Pain Management Strategies [10:06]
Pain management strategies include medication (non-steroidal anti-inflammatory drugs and paracetamol), with opioids used in severe cases (considering anti-doping regulations). Manual therapy, such as soft tissue mobilisation and joint manipulation, can be beneficial. Heat and cold therapy are used based on the healing phase. Physical medicine and rehabilitation (PMR) uses modalities to reduce inflammation and pain, manual therapy to restore mobility, and strength training to prevent reinjury. Neuromuscular retraining improves coordination and balance. Bracing and taping enhance proprioception and prevent excessive joint movement. Surgical interventions may be necessary for complete ligament rupture and severe tendon tears.
Return to Play Guidelines [12:55]
Return to play guidelines are based on pain-free function, strength, and sport-specific drills. Key considerations include whether the individual is pain-free, has regained strength relative to the non-affected limb, can complete sport-specific drills, and is psychologically ready. Workload should be increased gradually to prevent reinjury. Injury prevention strategies include proper warm-up and cool-down, appropriate load management, regular strength and conditioning, proper training techniques, correct footwear, and orthotics if needed. Early recognition of overuse injury signs is crucial.
Special Populations: Youth and Older Athletes [15:44]
Youth athletes may experience growth-related issues and are at higher risk for repetitive stress injuries. Training programs should be age-specific. Older athletes may have reduced tendon elasticity and slower recovery, requiring proper warm-up and mobility exercises. Preventive measures are more critical for older athletes to avoid chronic injuries.
Future Trends in Soft Tissue Injury Management [17:00]
Future trends include advances in regenerative medicine (platelet-rich plasma and stem cell therapy), wearable technology for injury prevention and load management, and artificial intelligence-based rehabilitation programs.
Take-Home Message [17:59]
The key takeaway is that common soft tissue injuries include strains, sprains, contusions, tendinopathies, and bursitis. Immediate care involves POLICE protocols for pain and swelling management. Rehabilitation includes gradual strengthening, mobility exercises, and physical therapy. Pain management may require non-steroidal anti-inflammatory drugs, manual therapy, and heat or cold applications. Return to play is only done after functional testing, scientific workload progression, and psychological readiness. Proper strength training, biomechanics, and early injury recognition are essential. Future trends involve regenerative medicine, AI-driven rehabilitation, and wearable technology for load management.