TLDR;
This video provides an overview of antidepressant drugs, their mechanisms of action, and their uses in treating depression and other psychiatric disorders. It covers the monoamine hypothesis, different classes of antidepressants (SSRIs, SNRIs, TCAs, MAOIs, and atypical antidepressants), and lithium as a mood-stabilizing drug. The video also discusses the side effects and drug-food interactions associated with these medications.
- Antidepressants work by elevating levels of certain neurotransmitters in the brain.
- The monoamine hypothesis suggests that depression results from a deficiency in serotonin, norepinephrine, and dopamine.
- Antidepressants are divided into five classes based on their mechanism of action: SSRIs, SNRIs, TCAs, MAOIs, and atypical antidepressants.
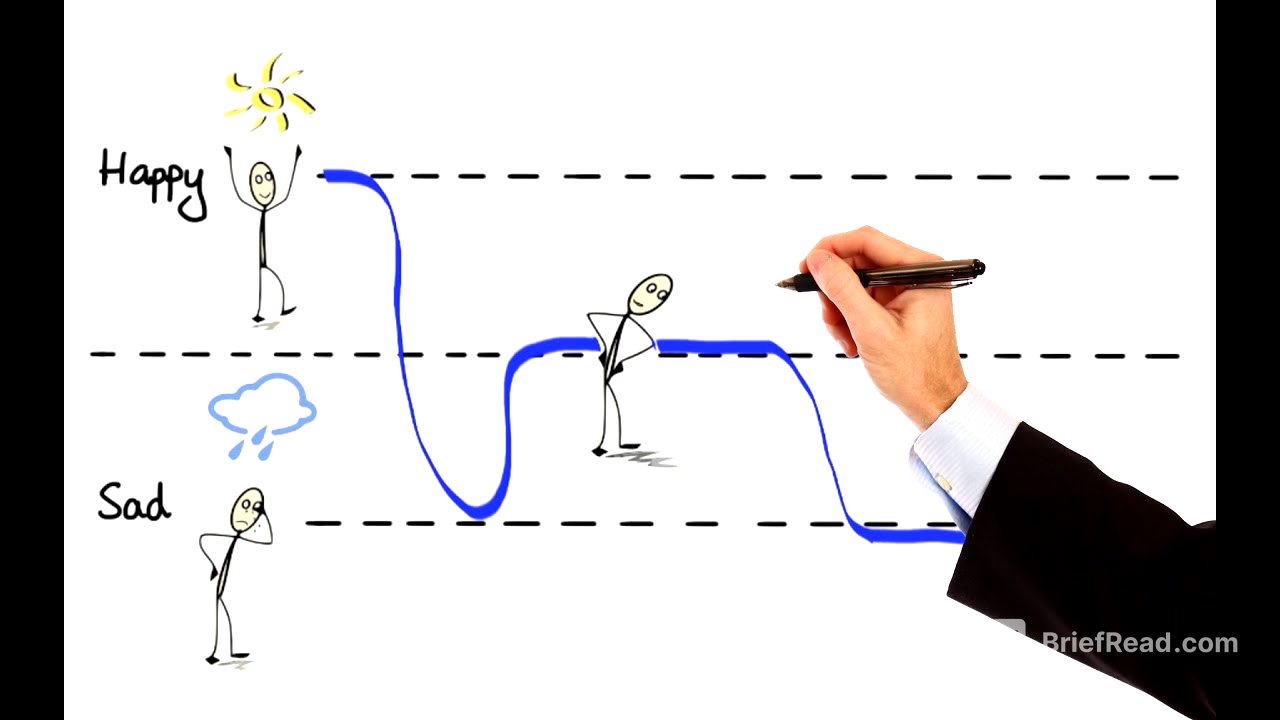
Monoamine Hypothesis [0:00]
The video introduces the concept of mood changes and how they relate to depression and bipolar disorder. Treatment for these conditions often involves antidepressant drugs, which work by increasing the levels of certain neurotransmitters in the brain. This leads to the monoamine hypothesis, which suggests that depression results from a deficiency in serotonin, norepinephrine, or dopamine. An alternative hypothesis suggests that monoamine depletion could cause postsynaptic receptors to upregulate, leading to depression. The monoamine hypothesis of gene expression proposes that an abnormal functioning gene might be responsible for causing depression.
Overview [1:55]
Based on their mechanisms of action, antidepressants are divided into five classes: selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), and atypical antidepressants. The following sections explain how these antidepressants differ in their mechanisms of action.
Serotonergic & Noradrenergic neurons [2:36]
The video describes the function of serotonergic and noradrenergic neurons. Serotonin, synthesized from tryptophan, is stored in vesicles within serotonergic neurons, while norepinephrine, synthesized from tyrosine, is stored in vesicles within noradrenergic neurons. When released, these neurotransmitters stimulate receptors and are then transported back into their respective neurons through a process called reuptake. Serotonin is reabsorbed by the serotonin transporter (SERT), and norepinephrine is reabsorbed by the norepinephrine transporter (NET). Once reabsorbed, serotonin and norepinephrine are partially repackaged into synaptic vesicles and partially broken down by the enzyme monoamine oxidase (MAO).
SSRIs [4:40]
Selective Serotonin Reuptake Inhibitors (SSRIs) block the serotonin transporter, increasing serotonin levels in the synapse. Examples include Citalopram, Escitalopram, Fluoxetine, Fluvoxamine, Paroxetine, and Sertraline. SSRIs are used for depression, generalized anxiety, post-traumatic stress disorder, and obsessive-compulsive disorder. SSRIs take weeks to produce maximum benefit because they gradually move G-proteins out of lipid rafts, allowing them to function better. Side effects include insomnia, increased anxiety, irritability, sexual side effects, nausea, vomiting, and diarrhea. Abrupt withdrawal can cause headache, nausea, vomiting, agitation, and sleep disturbances.
SNRIs [7:05]
Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) inhibit the reuptake of both serotonin and norepinephrine by blocking their respective transporters. Examples include Venlafaxine, Desvenlafaxine, Duloxetine, and Levomilnacipran. SNRIs are used for depression, anxiety, and panic disorders. They are also effective in reducing pain associated with fibromyalgia and neuropathy due to enhanced noradrenergic activity. Side effects are similar to SSRIs, but SNRIs may also increase blood pressure and heart rate due to increased noradrenergic activity.
TCAs [8:30]
Tricyclic Antidepressants (TCAs) inhibit the reuptake of both serotonin and norepinephrine, but with varying selectivity. Some TCAs, like Desipramine, are more selective for norepinephrine. TCAs also block alpha, histamine, and muscarinic receptors, contributing to their side effects. Examples include Amitriptyline, Amoxapine, Clomipramine, Desipramine, Doxepin, Imipramine, Maprotiline, Nortriptyline, and Protriptyline. TCAs are used for depression, migraine prevention (Amitriptyline and Nortriptyline), neuropathic pain (Amitriptyline and Nortriptyline), and insomnia (Doxepin). Side effects include orthostatic hypotension, dizziness, sedation, anticholinergic effects (blurred vision, dry mouth, constipation, urinary retention), and cardiac conduction abnormalities.
MAOIs [10:52]
Monoamine Oxidase Inhibitors (MAOIs) inhibit monoamine oxidase (MAO), an enzyme that degrades monoamines like serotonin and norepinephrine. MAO exists in two subtypes: A and B. Inhibition of MAO-A is thought to be responsible for the antidepressant effects. Examples include Isocarboxazid, Phenelzine, and Tranylcypromine, which are irreversible inhibitors of both MAO-A and MAO-B. Selegiline is a selective inhibitor of MAO-B and is used to treat Parkinson's disease. MAOIs are typically a last resort due to drug-drug and drug-food interactions. They can cause hypertensive crisis due to the build-up of tyramine from aged or fermented foods.
Atypical Antidepressants [13:44]
Atypical antidepressants have diverse mechanisms of action. Bupropion inhibits norepinephrine and dopamine reuptake and is also used to reduce nicotine cravings. Mirtazapine is an alpha-2 receptor antagonist, increasing noradrenergic and serotonergic neurotransmission, and has antihistaminic activity. Trazodone and Nefazodone inhibit serotonin reuptake and block postsynaptic serotonin 2A receptors, as well as antagonize histaminic H1 and adrenergic alpha-1 receptors. Vilazodone is a serotonin partial agonist reuptake inhibitor. Vortioxetine inhibits serotonin reuptake and modulates different serotonin receptor subtypes.
Lithium [16:07]
Lithium is a mood-stabilizing drug used primarily for bipolar disorder. It has a narrow therapeutic index, and its exact mechanism of action is not fully understood. One proposed mechanism involves inhibiting the recycling of neuronal membrane inositol lipids by inhibiting inositol phosphatase enzymes. Lithium also inhibits glycogen-synthase-kinase-3 (GSK3), mimicking the Wnt protein signaling pathway, which may contribute to its therapeutic effect. Lithium affects all major neurotransmitter systems in the brain.