TLDR;
This video features a presentation on controversies in manic depressive illness, focusing on diagnosis and treatment. The speaker critiques the DSM-based diagnostic approach, advocating for a non-DSM approach that considers mixed depression and mood temperaments. In terms of treatment, the speaker questions the validity of current research and emphasizes the potential benefits of lithium. The presentation challenges the audience to reconsider established practices in psychiatry and to adopt a more scientifically grounded and patient-centered approach.
- Critique of DSM-based diagnostic approach
- Advocacy for non-DSM approach considering mixed depression and mood temperaments
- Questioning the validity of current research
- Emphasis on potential benefits of lithium
Introduction [0:00]
The speaker introduces the topic of controversies in manic depressive illness, focusing on diagnostic approaches beyond the DSM and questioning current treatment research, particularly regarding lithium's benefits. He expresses his disillusionment with the psychiatric profession, stemming from interactions with DSM leaders and historical research. He directs the audience to resources, including books by historians Hannah Decker and Edward Shorter, and his own publications available on tmo.com, for further information on the historical context and his interpretations.
Critique of DSM and Historical Context [4:24]
The speaker discusses the historical context for the development of DSM-III, noting that it arose from a need to address chaos and anarchy in psychiatric diagnosis. Before the 1980s, psychoanalytic perspectives dominated, and definitive diagnoses were less critical. However, with the advent of new drugs in the 1960s and 70s, there was renewed interest in distinguishing between conditions like schizophrenia and mood disorders. Researchers, particularly those aligned with Kraepelinian ideas from Washington University in St. Louis, sought to validate diagnostic concepts using genetics, course of illness, biological markers, and treatment response.
The Development and Limitations of DSM-III [7:57]
The development of DSM-III grew out of research that aimed to validate definitions of schizophrenia and other disorders using genetics, course, outcome, and biological markers. However, the DSM-III criteria primarily included cross-sectional symptoms, omitting the course, genetics, and biology that informed their validation. The speaker argues that the DSM system has become overly reliant on symptoms, leading to an unscientific expansion of diagnoses. He claims that only a small percentage of DSM labels are supported by comprehensive evidence, with the majority based on pragmatic criteria, which are changes made based on what is considered best for the profession rather than on scientific evidence.
The Bipolar vs. Unipolar Distinction [12:12]
Before DSM-III, the concept of manic depressive illness encompassed various depressive presentations, including neurotic depression and melancholia. In 1980, DSM redefined these, relabeling most patients as having major depressive disorder (MDD) and only a small subset as bipolar. The key difference lies in the shift from "mania or depression" to "mania and depression." Manic depressive illness was defined by recurrent, severe, and episodic mood disturbances, regardless of polarity, whereas bipolar disorder requires both manic and depressive episodes.
Genetic and Research Evidence [16:29]
Genetic research indicates that bipolar patients inherit bipolar illness, while MDD patients primarily inherit unipolar depression. However, unipolar depression is genetically non-specific and can occur in families with bipolar illness. The speaker notes the issue of unipolar patients with bipolar family histories, which challenges the DSM system. He argues that MDD is a broad spectrum encompassing neurotic, melancholic, and mixed presentations. The speaker claims that the DSM leadership's pragmatism prevents the adoption of spectrum models due to concerns about diagnosing more patients and potential stigma.
The "Disorder" Concept and Postmodernism [21:46]
The speaker critiques the term "disorder" as explicitly vague and a way for the APA leadership to avoid committing to whether conditions are diseases. He argues that this approach is unscientific and driven by political, economic, and social considerations rather than biology. The speaker also discusses the influence of postmodernism, which promotes skepticism about science and truth, on DSM leaders, leading to a disregard for scientific expertise in defining diagnostic criteria.
Consequences of DSM System and Alternative Approaches [26:32]
The speaker argues that the DSM system dooms biological research to failure because its phenotypes are not scientifically valid. He suggests alternative approaches, such as returning to a smaller number of diagnoses, using a hierarchy concept instead of comorbidity, and treating patients with fewer medications. He also addresses the claim that bipolar disorder is overdiagnosed, particularly in children, and presents evidence suggesting underdiagnosis instead.
Bipolar Disorder in Children and Adults [31:37]
The speaker addresses the misconception that bipolar disorder is overdiagnosed, especially in children. He presents data indicating that bipolar illness in children often manifests as depression, with manic episodes developing later. He cites studies showing that a significant percentage of severely depressed young adults eventually develop manic episodes. The speaker also critiques studies claiming overdiagnosis of bipolar disorder in adults, arguing that their own data reveal underdiagnosis.
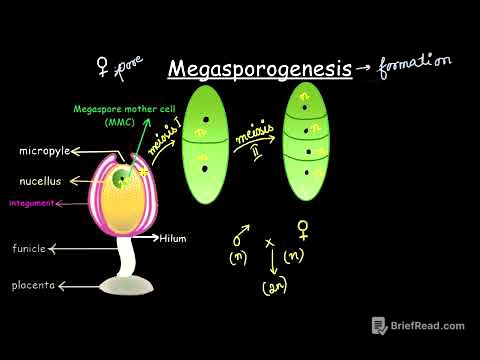
Mixed Depression [37:46]
The speaker discusses the concept of mixed depression, emphasizing broader definitions beyond the narrow criteria in the DSM system. He highlights the definitions of mixed depression by Cucopulos, characterized by depression mixed with psychomotor excitation, and Angst, defined by brief periods of manic symptoms. Research indicates that mixed states are common in mood episodes, confirming Kraepelin's view that most patients are mixed rather than purely manic or depressed.
Therapeutic Implications of Mixed Depression and Mood Temperaments [42:25]
The speaker discusses the therapeutic implications of mixed depression, noting that dopamine blockers may be helpful for agitated mixed depression, while antidepressants may be harmful. He emphasizes the importance of recognizing mixed depression to avoid inappropriate antidepressant use, which can worsen agitation and suicidality. The speaker also introduces the concept of mood temperaments, such as cyclothymia, hyperthymia, and dysthymia, as mild versions of mood disorders that can influence personality and behavior.
Mood Temperaments and ADHD [45:27]
The speaker discusses mood temperaments, such as hyperthymia and cyclothymia, and their potential misinterpretation as adult ADHD. He questions the belief that ADHD is purely biological and persistent, citing studies showing a decline in ADHD rates by young adulthood and state-to-state differences in ADHD diagnoses. He suggests that environmental factors play a significant role in ADHD, similar to heart disease.
Treatment: Terminology and Hypocratic Approach [54:46]
The speaker critiques the terms used for psychiatric drugs, such as "antipsychotic," "mood stabilizer," and "antidepressant," and suggests using biological mechanisms instead. He introduces a hypocratic approach to treatment, emphasizing the importance of treating diseases rather than just symptoms. He argues that many patients present with symptoms but do not have a disease, and in such cases, treatment should be minimal to avoid harm.
Treatment: Maintenance Studies and Amphetamines [1:02:10]
The speaker critiques the study designs used to support long-term drug treatments, particularly randomized discontinuation trials, which he argues are inherently biased. He also raises concerns about the use of amphetamines, citing their potential neurotoxic effects and the risk of misinterpreting mood temperaments as ADHD.
Treatment: Antidepressants and Lithium [1:08:45]
The speaker expresses strong reservations about the use of antidepressants, citing meta-analyses and his own research indicating limited benefit and potential harm, especially in mixed depression. He advocates for caution with antidepressants and suggests considering ECT for severe depression. The speaker also highlights the benefits of lithium, including its effectiveness in preventing depression, dementia, and suicide.
Conclusion [1:12:53]
The speaker summarizes the need to move beyond the DSM framework, think more scientifically, and consider concepts like mixed depression and mood temperaments. He encourages critical evaluation of treatment designs and emphasizes the potential benefits of lithium. The presentation concludes with a video clip of Martin Luther King Jr. discussing the importance of being maladjusted to injustice, suggesting that functional impairment may have social benefits.