TLDR;
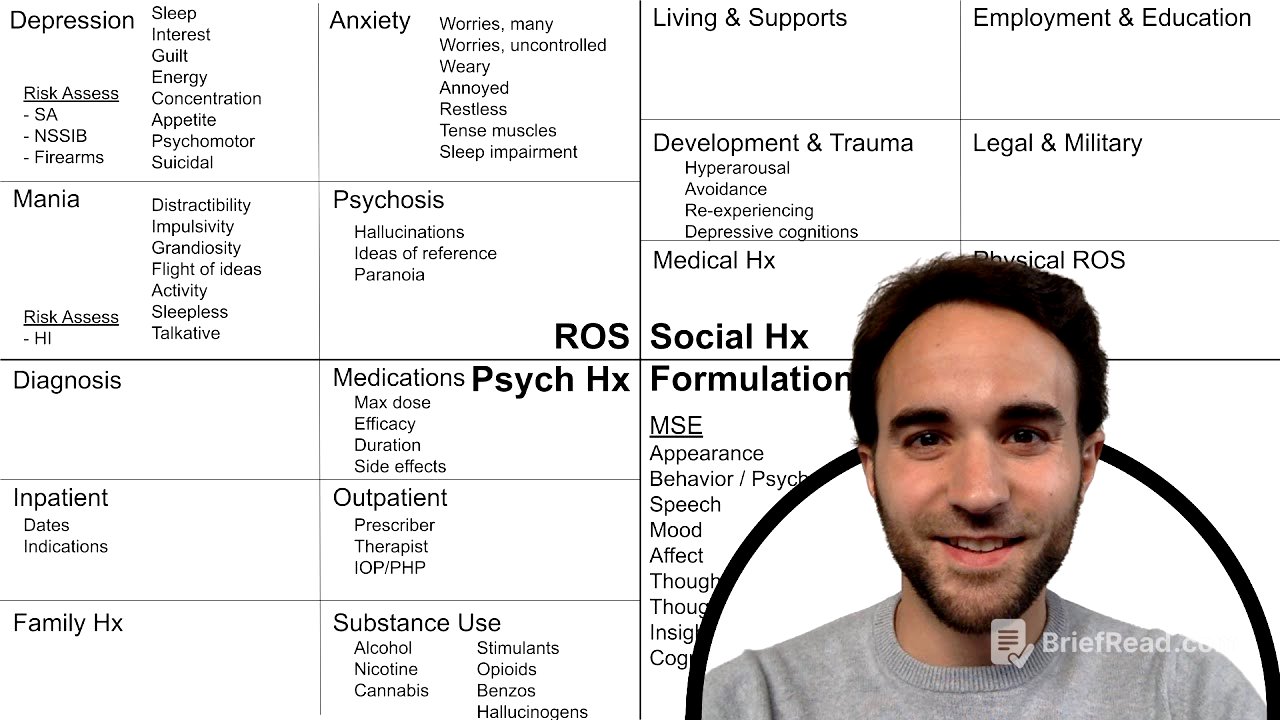
This video provides a structured approach to conducting an initial psychiatric history interview. It uses a visual organizer with four key components: psychiatric review of symptoms, psychiatric history, social history, and formulation. The video offers pneumonics and key questions to guide each section, ensuring a thorough and compassionate interview.
- Psychiatric Review of Symptoms: Uses "DAMP" (Depression, Anxiety, Mania, Psychosis) to guide symptom inquiry.
- Psychiatric History: Explores prior diagnoses, medication trials (using "MEDS"), and past treatments.
- Social History: Covers living situation, social supports, employment, education, and trauma history (using "HARD" for trauma-related symptoms).
- Formulation: Dedicated space for mental status exam notes, diagnostic ideas, and treatment plans.
Introduction [0:00]
The video introduces a method for conducting an initial psychiatric history interview using a visual organizer. The organizer includes four major components: the psychiatric review of symptoms, psychiatric history, social history, and formulation. It excludes the history of present illness, which should be completed before this part of the interview.
Psychiatric Review of Symptoms [0:28]
This section focuses on four symptom clusters, represented by the mnemonic "DAMP": Depression, Anxiety, Mania, and Psychosis. For depression, the mnemonic "SIG E CAPS" is used to explore symptoms of a major depressive episode, including assessing suicide risk factors like prior attempts, non-suicidal self-injury, and access to firearms. For anxiety, the mnemonic "Worry Warts" guides the assessment of generalized anxiety disorder, along with inquiries about panic attacks. Mania is assessed using "DIG FAST" to identify symptoms of a manic episode, and this is also a time to screen for homicidal ideation. For psychosis, the focus is on hallucinations and common delusions like ideas of reference and paranoia, supplementing information gathered from the mental status exam regarding disorganized thinking, behavior, and negative symptoms.
Psychiatric History [1:41]
In this section, the interviewer should inquire about prior psychiatric diagnoses and medication trials. The mnemonic "MEDS" is used to gather information about prior medication trials, including the maximum dose, efficacy, duration of treatment, and any side effects. The interviewer should also ask about past inpatient and outpatient psychiatric treatments, including dates of admission, indications for admission, prescribers, therapists, and participation in intensive outpatient or partial hospital programs. Finally, the interviewer should ask about family history of mental illness and any past or current substance use issues.
Social History [2:48]
The social history section covers the patient's living situation, social supports, employment and education history, and developmental and trauma history. In initial interviews, it's advised to screen for major categories of trauma—physical, sexual, and emotional—without pressing for sensitive details. Trauma-related symptoms are assessed using the mnemonic "HARD". Additionally, legal and military history, a brief medical history (including chronic illnesses, current medications, and allergies), and a physical review of systems should be included.
Formulation [3:51]
This section is reserved for the interviewer to record notes from the mental status exam, diagnostic ideas, and the patient's treatment plan. The video emphasizes the importance of flexibility in structuring the interview, adapting to the patient's needs, and developing a thorough, concise, and compassionate interviewing style over time.