TLDR;
This video introduces integrative psychiatry as a holistic approach to mental health that seeks to identify and address the root causes of psychiatric symptoms, rather than merely treating the symptoms themselves. It contrasts conventional psychiatry's focus on symptom clusters and pharmaceutical interventions with integrative psychiatry's comprehensive evaluation, consideration of lifestyle and environmental factors, and expanded toolkit of treatments. The video highlights the increasing global burden of mental illness and the limitations of current treatment models, suggesting that integrative psychiatry may offer a more effective and sustainable alternative.
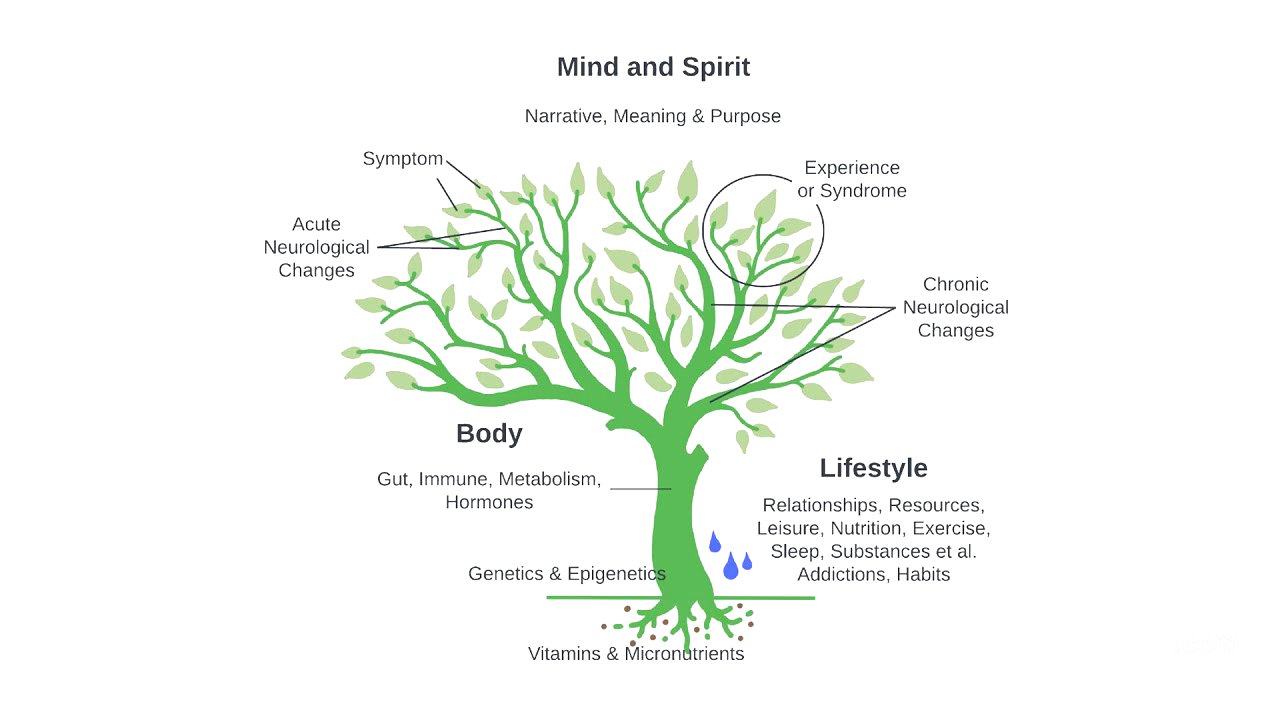
- Integrative psychiatry explores mind, body, lifestyle, and spirituality to identify root causes of psychiatric symptoms.
- Conventional psychiatry focuses on symptom reduction with pharmaceutical options, while integrative psychiatry expands the toolkit to include nutraceuticals and alternative treatments.
- The goal is to consider the whole person rather than just sorting through the leaves (symptoms).
Introduction to Integrative Psychiatry [0:18]
Integrative psychiatry is introduced as a comprehensive approach that explores the whole person to identify the root causes of psychiatric symptoms and experiences. This exploration includes mind, body, lifestyle, and spirituality. The video uses the metaphor of a tree to illustrate this approach, where leaves represent individual symptoms, branches represent neurological changes, the trunk represents bodily systems, and the roots represent genetic and epigenetic factors. Lifestyle factors are depicted as water that can either help or hinder growth, while mind and spirit surround the tree, informing an individual's narrative and purpose.
The Growing Burden of Mental Illness [1:52]
The global burden of mental illness is highlighted, noting a significant increase in disability-adjusted life years due to mental illness between 1990 and 2019. Mental health disorders remain among the top 10 leading causes of burden worldwide, with no evidence of reduction since 1990. Depression is identified as the leading cause of disability worldwide and is predicted to be the leading cause of global burden of disease by 2030. A significant portion of individuals who need mental health services lack access to care, and for those who do receive care, pharmacological treatments may not always be effective, with some studies showing small effect sizes or equivalence to placebo.
Limitations of Conventional Psychiatry [2:56]
Discrepancies in conventional psychiatric treatment are discussed, including long-term outcome issues and treatment resistance. Despite one in five adults in the United States experiencing a mental illness, the current model may not be the most effective for addressing this growing issue. Conventional psychiatry focuses on syndromes and symptom clusters, which can be stigmatizing, and often relies on a checklist approach to identify a diagnosis based on an idiopathic cluster of symptoms. This labeling can be misleading as it is unlinked from etiology and stigmatizing.
Integrative Psychiatry as an Alternative [3:27]
Integrative psychiatry is presented as a more effective alternative to the current model, focusing on root causes rather than just symptom reduction. While conventional psychiatry orients treatment around symptom reduction with a heavy reliance on pharmaceutical options, integrative psychiatry expands this toolkit to include nutraceuticals and other alternative treatments aimed at root causes. The role of the practitioner in integrative psychiatry is more of a guide, presenting both in-the-box and out-of-the-box options and allowing the patient to make an informed and autonomous decision. The course will examine a variety of modalities guided by an integrative model of treatment, incorporating relevant evidence-based support to address the root causes of mental illness and consider the whole person.