TLDR;
This lecture provides an overview of electrical stimulation and ultrasound therapies in sports rehabilitation, emphasizing their therapeutic effects, rational use, and application in different phases of tissue healing. It highlights the shift towards active, technology-integrated, and evidence-based practices, focusing on pain relief, muscle strengthening, inflammation reduction, and tissue healing. The lecture also covers specific types of electrical stimulation, ultrasound modes, and their mechanisms of action, along with precautions and best practices for their use.
- Electrical stimulation and ultrasound therapies are effective, non-invasive treatments for musculoskeletal conditions.
- These modalities improve tissue healing, reduce pain, and enhance muscle function.
- Integrating these therapies into sports rehabilitation, based on the phase and rehabilitation goal, improves patient outcomes and complements exercise therapy.
Introduction [0:16]
The lecture addresses how electrical stimulation and ultrasound modalities can improve sports rehabilitation outcomes and aid in early return to play, using the example of Raini, a volleyball player with a knee injury. It introduces the course on physical medicine and rehabilitation in sports, focusing on therapeutic modalities. The learning objectives include understanding the need for aligning sports injury rehabilitation phases with the therapeutic effects of electrical stimulation and ultrasound therapy, discussing the rationale for their use, and applying these concepts in a practical scenario.
Changing Paradigms in Sports Physical Therapy [1:57]
The field of physical therapy, especially in sports, is shifting from passive care to active, technology-integrated protocols with an evidence-based approach centered on the athlete. It's crucial to align therapeutic modalities with tissue healing principles, which involve three phases: the acute inflammatory phase (3-7 days), the proliferative phase (1-3 weeks), and the remodeling phase (extending up to months or years). Rehabilitation goals should align with these phases, focusing on controlling damage and inflammation in the acute phase, restoring function in the subacute phase, and returning to sport with reinjury prevention in the later phases.
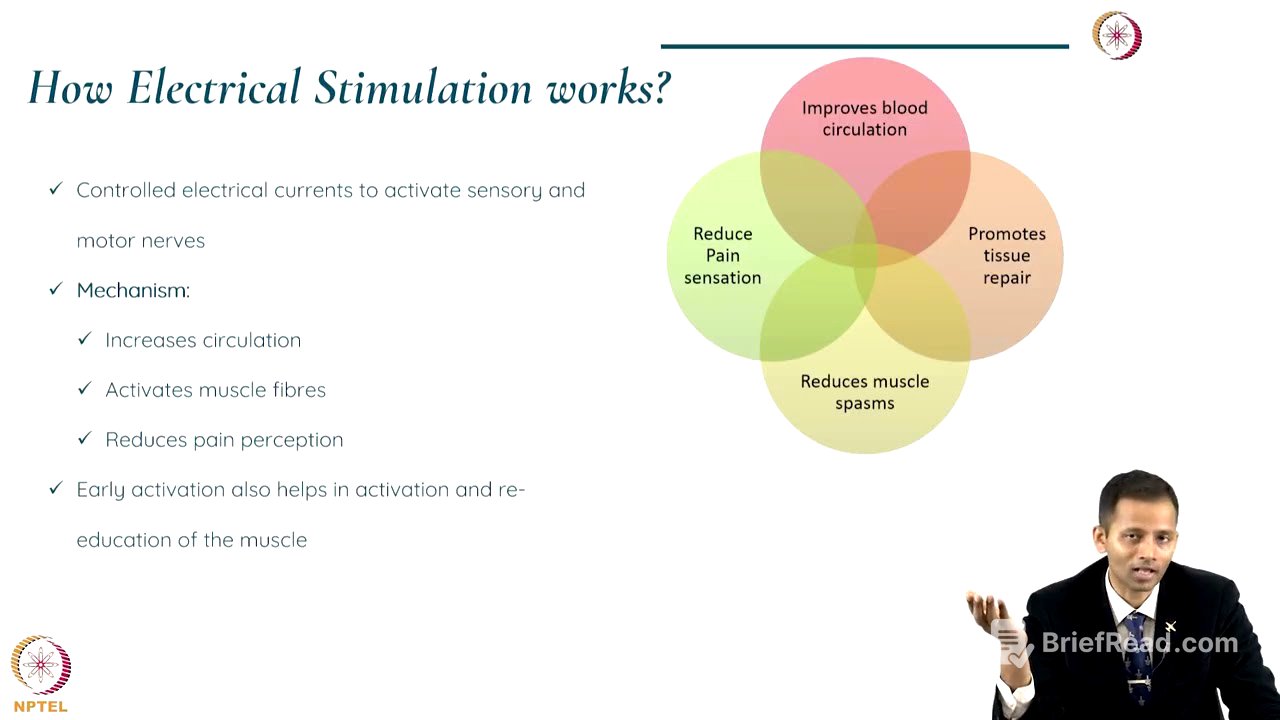
Electrical Stimulation Modalities [6:20]
Electrical stimulation uses controlled electrical currents to stimulate nerves and muscles, relieving pain, reducing inflammation, and promoting healing. Transcutaneous Electrical Nerve Stimulation (TENS) is used for pain relief, while Neuromuscular Electrical Stimulation (NMES) stimulates muscles. By activating sensory or motor nerves, these modalities increase circulation, activate muscle fibers, and reduce pain perception and muscle spasms. Types of electrical stimulation include TENS for pain modulation, NMES for muscle strengthening, Interferential Currents (IFC) for pain relief and muscle stimulation, and electrical muscle stimulation for re-educating muscles.
Applications and Benefits of Electrical Stimulation [8:36]
Electrical stimulation is used in sports rehabilitation to manage pain in both acute and chronic injuries, strengthen muscles weakened by disuse or post-surgery, and reduce inflammation and promote tissue healing by reducing spasms and improving circulation. It is a non-invasive modality that reduces pain and spasms, improves healing, reduces inflammation, and enhances circulation, complementing exercise therapy and improving strength.
Case Study: Volleyball Player with Knee Injury [9:58]
In the case of the volleyball player with a knee injury, electrical stimulation modalities can be used in different phases of rehabilitation. In phase one, cryotherapy and interferential therapy (IFT) can reduce pain and swelling. In phase two, IFT can continue for swelling and pain, while neuromuscular electrical stimulation can activate the vastus medialis obliquus muscle, which is prone to inhibition due to inflammation and pain. This helps in re-educating the muscle and can be combined with isometric and concentric exercises. TENS can also be used for pain relief around the knee.
Ultrasound Therapy [12:19]
Ultrasound therapy uses high-frequency sound waves to promote tissue healing, applicable to both superficial and deep tissues, with frequencies of 3 MHz for superficial and 1 MHz for deeper effects. There are two types of ultrasound: thermal and non-thermal. Thermal ultrasound uses 1 MHz frequency for deeper tissues, promoting circulation and muscle relaxation, while non-thermal ultrasound uses 3 MHz for superficial tissues, promoting cellular repair and reducing inflammation. Modes include continuous (similar to diathermy) and pulsed, which has different effects based on therapeutic goals.
Mechanism of Action and Applications of Ultrasound [14:14]
The mechanism of action involves a crystal in the applicator that produces mechanical sound waves through the piezoelectric effect, transmitted to the tissue via ultrasound gel. Thermal effects in deeper tissues increase blood flow, cellular metabolism, and decrease spasm, while non-thermal effects at the superficial level promote cellular repair, increase fluid movement, and decrease inflammation and pain. Ultrasound can be used in acute soft tissue injuries, joint injuries, chronic inflammation, tendinopathies, scars, non-healing ulcers, and bone injuries, including stress fractures where low-intensity pulsed ultrasound (LIPUS) can promote faster healing.
Benefits and Future Trends [16:57]
Ultrasound therapy can be used in both acute and chronic conditions, for superficial and deep tissues, accelerating healing by promoting collagen production and reducing pain, spasm, and stiffness. It provides deep heating without tissue damage and can be combined with other therapies. Future trends include more portable and user-friendly equipment, such as hands-free ultrasound, and integration with biofeedback and virtual/augmented realities for muscle re-education. Individualized and patient-specific treatment plans are emphasized, requiring a sound scientific rationale and evidence-based practice.
Precautions, Contraindications, and Best Practices [18:29]
Precautions and contraindications for electrical stimulation include avoiding use in pregnant uteri, patients with pacemakers, and open wounds with cancerous regions. Correct electrode placement is crucial, and monitoring for skin irritation and burns is important. For ultrasound therapy, contraindications include pregnancy, cancer, deep vein thrombosis, and infections. Choosing the right mode and frequency is essential to prevent tissue damage or burns. Best practices include using proper electrodes, skin preparation, starting with low intensity, and tailoring frequency, pulse, and duration based on patient response. For ultrasound, select the right frequency and duration, move the head slowly in a circular motion, and ensure adequate gel contact.
Summary [22:19]
Electrical stimulation and ultrasound therapy are effective, non-invasive treatments for musculoskeletal conditions, improving tissue healing, reducing pain, and enhancing muscle function. Integrating them into sports rehabilitation based on the phase and rehabilitation goal improves patient outcomes and complements exercise therapy. These modalities modulate pain and inflammation, enhancing adherence to exercise therapy.